No products in the cart.
Manager, Underwriter (Senior Underwriting Consultant) – WFH Flexible
0
This listing has expired.
OPERATING HOURS
Online all the time
Office Hours: 8 AM to 8 PM
Office Hours: 8 AM to 8 PM
Sitemap | Published Press | Privacy Policy
Staff Email | Independent Media | Buy traffic for your website | Change privacy settings
OPERATING HOURS
Online all the time
Office Hours: 8 AM to 8 PM
Sitemap | Published Press | Privacy Policy
Staff Email | Independent Media
Buy traffic for your website
Change privacy settings
Office Hours: 8 AM to 8 PM
Sitemap | Published Press | Privacy Policy
Staff Email | Independent Media
Buy traffic for your website
Change privacy settings
LIVE WEBSITE VIEWERS
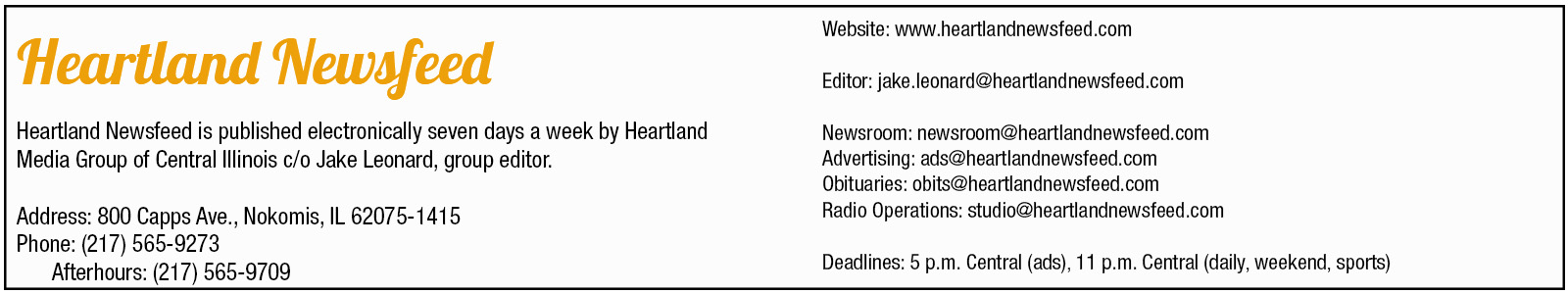
Some rights reserved 2017-2024 by Heartland Newsfeed, a Heartland Media Group of Central Illinois media property. Content published by Heartland Newsfeed staff is covered by the BipCot NoGov license. This allows use and re-use by anyone except governments and government agents. License on record. JNews theme designed and developed by Jegtheme.

